Rare Axilla-Positive Subcentimetric Breast Cancer Treated With BCS & Flap At RG Hospitals, Rajouri Garden
Faculty:
Dr. Neerja Gupta (Senior Consultant – Breast Surgical Oncology)
A 73-year-old female presented with vague symptoms of redness around the left nipple off and on with itching.
MRI revealed diffuse enhancement in the outer quadrant of the left breast.
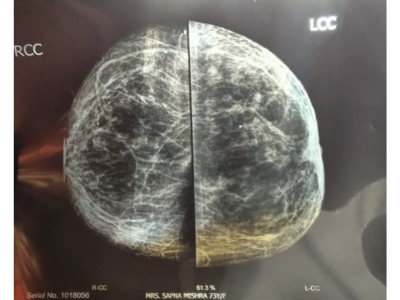
Mammogram showed no lesion or calcification.
A second opinion on MRI identified three suspicious foci of 0.5–0.6 cm.
Biopsy of one 5 mm nodule confirmed invasive ductal carcinoma; staging was negative.
Diagnosis:
Invasive Ductal Carcinoma of the Left Breast (Multifocal)
Staging:
PET CT with contrast
Treatment Performed:
Left Breast Conserving Surgery (BCS)
Rotation Flap Reconstruction
Sentinel Lymph Node Biopsy – Frozen Section Positive
Completion Axillary Lymph Node Dissection
Key Highlights of the Case:
Tumor resection performed in standard anatomical planes – from subcutaneous tissue to pectoral fascia
BCS specimen sent for frozen section to assess radial resection margins
Rotation flap used for breast reconstruction to maintain shape and volume
Sentinel node positive on frozen, followed by full axillary clearance
No bleeding; hemostasis secured
Patient tolerated the procedure well with stable intraoperative vitals
Postoperative course was smooth; patient was managed with IV antibiotics, fluids, antiemetics, and supportive care
Final HPE:
Three nodules – 5 mm, 5 mm, and 6 mm in the resected specimen; largest tumor diameter 6 mm; all margins free; IDC Grade III
This case is a testament to RG Rajouri Garden’s commitment to organ-preserving breast cancer surgery with oncological safety and aesthetic precision. By combining breast-conserving techniques with effective lymph node management and flap-based reconstruction, the team ensured a functional, oncological, and cosmetic outcome tailored to the patient's age and condition.
The case highlights challenges in impalpable lesions presenting as nodules of less than 1 cm, accurately localized through close clinician–radiologist coordination, enabling wide excision with clear margins on both frozen and final HPE.