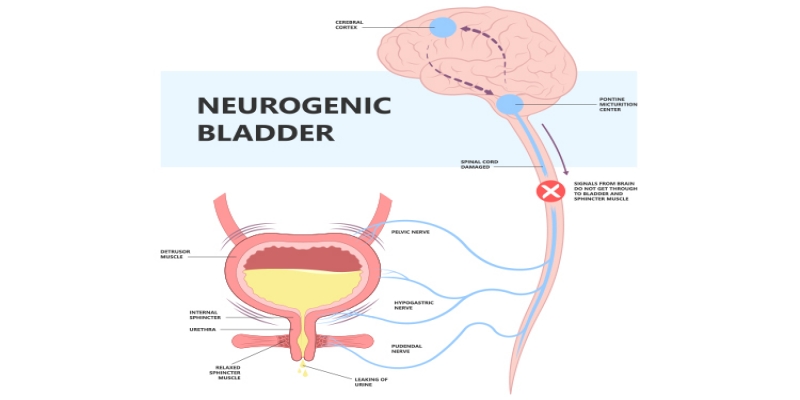
Neurogenic bladder is a urinary dysfunction caused by damage to the nervous system that controls bladder function. The primary causes include spinal cord injuries, multiple sclerosis, Parkinson's disease, diabetic neuropathy, and congenital conditions like spina bifida. Brain injuries, strokes, and certain surgeries can also lead to neurogenic bladder. Symptoms vary depending on the location and extent of nerve damage, but generally fall into two categories: overactive bladder (frequent, urgent urination) or underactive bladder (difficulty emptying the bladder completely). Patients may experience urinary incontinence, urinary retention, frequent urinary tract infections, and in severe cases, damage to the kidneys due to high bladder pressures. Some individuals may have a combination of both overactive and underactive symptoms, leading to complex urinary dysfunction.
Procedures & Interventions
Intermittent or indwelling catheterization is often used to manage urinary retention and prevent complications. Patients or caregivers are trained in proper catheterization techniques.
Various drugs can be prescribed to manage symptoms. Anticholinergics may help reduce bladder overactivity, while alpha-blockers can relax the bladder neck and urethra to improve emptying.
Injections of botulinum toxin into the bladder muscle can help reduce overactivity and improve bladder capacity. Effects typically last several months before needing repeat treatment.
Techniques like sacral nerve stimulation can help regulate nerve signals controlling bladder function. This may involve implanted devices for long-term management.
Timed voiding, double voiding, and pelvic floor exercises may be taught to improve bladder control and emptying. These are often used in conjunction with other treatments.
In severe cases, surgical options may include bladder augmentation to increase capacity, creation of a continent urinary diversion, or placement of an artificial urinary sphincter.
External or implanted devices can be used to stimulate nerves and muscles involved in bladder control, potentially improving function.
Treating the underlying neurological condition, when possible, is crucial for overall management of neurogenic bladder.
These may include fluid management, dietary changes, and techniques to prevent urinary tract infections.

Intermittent or indwelling catheterization is often used to manage urinary retention and prevent complications. Patients or caregivers are trained in proper catheterization techniques.

Various drugs can be prescribed to manage symptoms. Anticholinergics may help reduce bladder overactivity, while alpha-blockers can relax the bladder neck and urethra to improve emptying.

Injections of botulinum toxin into the bladder muscle can help reduce overactivity and improve bladder capacity. Effects typically last several months before needing repeat treatment.

Techniques like sacral nerve stimulation can help regulate nerve signals controlling bladder function. This may involve implanted devices for long-term management.

Timed voiding, double voiding, and pelvic floor exercises may be taught to improve bladder control and emptying. These are often used in conjunction with other treatments.

In severe cases, surgical options may include bladder augmentation to increase capacity, creation of a continent urinary diversion, or placement of an artificial urinary sphincter.

External or implanted devices can be used to stimulate nerves and muscles involved in bladder control, potentially improving function.

Treating the underlying neurological condition, when possible, is crucial for overall management of neurogenic bladder.

These may include fluid management, dietary changes, and techniques to prevent urinary tract infections.
Team of Excellence
Behind every recovery story at RG Hospitals is a team of exceptional doctors whose passion for healing and innovation continues to transform healthcare and redefine patient outcomes.
Find a DoctorLooking for an Expert
RG Hospitals is proud to be the home of some of the world's most distinguished doctors.

Patient Stories
View AllPatient Testimonial | Commitment To Care
Treated by Dr. Manoj Gupta , RG Stone Hospital, Dehradun
- All Locations
- New Delhi
- Haryana
- Punjab
- Kolkata
- Chennai
- Mumbai
- Goa
- Uttar Pradesh
- Uttarakhand